What Are Training Adaptations to Continued Endurance Exercise Explain Physiologically
Original Editor - Nadja Thöner
Top Contributors - Wendy Walker, Lucinda hampton, Tarina van der Stockt, Admin, Kim Jackson, Tony Lowe, Michelle Lee, Ewa Jaraczewska, Nikhil Benhur Abburi, Chelsea Mclene, Evan Thomas, Naomi O'Reilly, Shaimaa Eldib, Rucha Gadgil and Wanda van Niekerk
Introduction [edit | edit source]

Compared to our resting state, exercise poses a substantial increase in demand for the body.
- At rest, our nervous system maintains a parasympathetic tone which affects the respiratory rate, cardiac output, and various metabolic processes.
- Exercise stimulates the sympathetic nervous system and will induce an integrated response from the body.
- This response works to maintain an appropriate level of homeostasis for the increased demand in physical, metabolic, respiratory, and cardiovascular efforts[1]
- Exercise challenges many human physiological systems that need to adapt in order to maintain homeostasis, this is the inner balance of the body.
- While exercising, homeostasis is endangered by the increased amount of O2 and nutrients demand, the need to get rid of CO2 and metabolic waste products, rising body temperature and acid imbalance and varying hormone levels.
Function [edit | edit source]
Exercise has been shown to have many health benefits. Through functional exercise, we can see benefits in but not limited to:
- Cognition: Studies have shown exercising subjects to have higher concentration scores than non-exercising subjects.
- Flexibility and mobility
- Cardiovascular health
- Improved glycemic control and insulin sensitivity
- Mood elevation
- Lower risks of cancer
- Increased bone mineral density
Through a properly executed exercise program, the body adapts and becomes more efficient at performing various exercises.[1]
These adaptations are acute and/or chronic
1. Acute Adaptations to Exercise [edit | edit source]
Cardiovascular Responses [edit | edit source]
To accommodate the increased metabolic activity in skeletal muscle, the circulatory system must properly control the transport of oxygen and carbon dioxide, as well as help to buffer the pH level of active tissues.
- This is accomplished by increasing cardiac output (increased heart rate and stroke volume) and modulating microvascular circulation.
- In addition, the action of local vasodilators such as nitric oxide from endothelial cells helps to ensure adequate blood flow.
1. Cardiac Output (Q) [edit | edit source]
- The amount of blood pumped by the left ventricle per minute is expressed as litres/minute. Q = (HR) X stroke volume (SV).
- With a stepping working rate, the cardiac output increases in a nearly linear fashion in order to meet the increased oxygen demand.
- Cardiac output is measured by echocardiography.
VO2 is the consumption of oxygen and can be explained by the Fick equation.
This equation states that VO2 = [CardiacOutput] x [Difference in arterial and venous oxygen levels].
VO2max is a measure of aerobic exercise capacity and is defined as the highest rate of oxygen uptake an individual can maintain during intense activity.[1]
- At rest, the value is on average about 4-5 mL/100mL of blood and
- can raise progressively during an exercise up to 16 mL/100mL of blood (4).
The 4-minute video below explains the A-V02 difference
Blood flow is preferentially shunted away from the gastrointestinal (GI) and renal systems and toward active muscles through the selective constriction and dilation of capillary beds with increasing physical stress,[1]
- at maximal rates of work, 80 per cent of the cardiac output goes to the activated muscles and the skin
- in rest, this value is just twenty per cent.
2. Blood Pressure [edit | edit source]
There is a linear increase in systolic blood pressure to peak values of 200 to 249 mmHg in normotensive individuals, and the diastolic pressure value remains near rest level.
- Hypertensive individuals reach higher systolic blood pressures at a given rate of work, and they can also reach higher diastolic values.
- The peripheral resistance of blood flow is related to vessel diameter and length and blood viscosity in the peripheral vessels.[2]
- Under physical demands the vessels dilate, increasing their diameters.
- Hypertension patients have increased peripheral resistance compared to normal, and this is a major cause of their higher average blood pressure.
Two to three hours post-exercise blood pressure drops below pre-exercising values, this is known as "post-exercise hypotension".
3. Coronary Circulation [edit | edit source]
Coronary arteries supply the myocardium with blood and nutrients; on average one capillary supplies one myocardial fibre in the ventricular walls and papillary muscles.[3]
Pulmonary System Adaptations [edit | edit source]
Pulmonary ventilation is initiated via the respiratory centre in the brainstem with parallel activation through the motor cortical drive that activates skeletal muscles and afferent Type III-IV muscle afferent fibres.
The respiratory system works in junction with the cardiovascular system. The pulmonary circuit receives almost all of the cardiac output. In response to the increased cardiac output, perfusion increases in the apex of each lung, increasing the available surface area for gas exchange (decreased alveolar dead space).
Maximum exercise training ventilation rates in normal-sized healthy people may increase by a factor of ten, compared to ventilation rates at rest
Musculoskeletal System [edit | edit source]
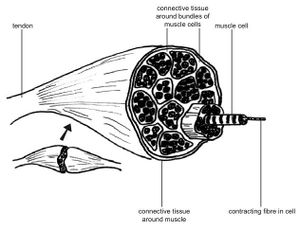
There are 3 types of muscle fibers which have different characteristics.
Type-I fibres are known as slow-twitch fibres. These fibres have abundant mitochondria and myoglobin with great vascular supply.
- They have: Low myosin ATPase activity, High oxidative, Low glycolytic capacity
- These fibres are predominant in postural muscles as they provide low force but don't fatigue as easily as the others.
Type-IIa fibres are known as fast-twitch oxidative fibres.
- They have: High myosin ATPase activity, high oxidative, high glycolytic capacity
- Relatively resistant to fatigue
- These fibres are recruited for power activities that require sustained effort such as weight lifting for multiple repetitions.
Type-IIa fibres can be considered as the middle-ground type of fibre, between the slow but fatigue-resistant type-I fibres and the fast but fatigue-prone type-IIb fibres.
Type IIb fibres are known as fast-twitch glycolytic fibres.
- They have high myosin ATPase activity, low oxidative, high glycolytic activity.
- Rapidly fatigue
- These fibres are recruited for high intensity, short-duration exercises such as full effort sprints.
With the introduction of progressively overloading exercise training, we can expect skeletal muscle fibres to hypertrophy meaning they increase in diameter and volume.
- Muscle contraction acts upon the skeleton and initiates movement. When a progressive force is applied to the muscles over time, they will adapt to the increasing load.
- Satellite cells play a role in this repair and growth process.
- The process of exercise (eg long-distance running or powerlifting) places a burden of stress on muscle fibres and bones which causes micro-tears and trauma.
- In response to this, satellite cells are activated and mobilized to regenerate damaged muscle tissue.
- This process is made possible by the donation of daughter nuclei from the satellite cells after multiplication and fusion.
- The bones will increase their mineral density over time to manage this increasing load.[1]
Resistance Exercise [edit | edit source]
Dynamic training and strength training differ primarily in the fact that resistance training produces a vigorous increase in peripheral vascular resistance.
- Strength training, high isolated forces generated in the activated musculature which compresses the small arteries and thus increases the peripheral vascular resistance.[4]
Skeletal Muscle Fibre Type [edit | edit source]
The type of physical exercise being undertaken determines the predominant muscle fibre type.
Endurance Training ( regular) [edit | edit source]
- Increases the number of mitochondria and the gas exchange capacity of the trained myofibrils.
- In marathon runners, slow-twitch fibres dominate the trained leg muscles (while sprinters possess predominantly fast-twitch fibres).
- has the potential to change the metabolic properties of skeletal muscles in the direction of an oxidative profile. The question as to how far muscle fibre types can be reprogrammed remains open.
Hormonal Responses to Exercise [edit | edit source]
Endocrine System [edit | edit source]
Plasma levels of cortisol, epinephrine, norepinephrine, and dopamine increase with maximal exercise and return to baseline after rest.
- The increase in levels is consistent with the increase in sympathetic nervous system activation of the body.
- Growth hormone is released by the pituitary gland to enhance bone and tissue growth.
- Insulin sensitivity increases after long-term exercise.
- Testosterone levels also increase leading to enhanced growth, libido, and mood
- Catecholamines are part of cardiovascular and respiratory training adaptations and in fuel mobilisation and utilisation.
Immunological Adjustments [edit | edit source]
Moderate training enhances some components of the immune system and thereby reduces the susceptibility to infections. In contrast, reduced functionality of immune cells occurs after overstraining.
2. Chronic Adaptations of Exercise [edit | edit source]
Skeletal Muscle Adaptations [edit | edit source]

1. Endurance Training [edit | edit source]
Slow-twitch fibres: The cross-sectional area of slow-twitch (AKA red) fibres increases slightly in response to aerobic work.
Fast-twitch fibres: These fibres develop a higher oxygen capacity.
Capillary bed density: Trained muscles possess a higher density of capillaries than untrained muscle, which permits a greater blood flow with increased delivery of nutrients.
2. Resistance/ strength Training [edit | edit source]
Resistance training causes increased muscle size (hypertrophy) through an increase of myofibril size and the number of fast- and slow-twitch fibres. Moreover, the recruitment pathway of muscle fibres become more effective. Resistance training thus leads to greater force development of the trained muscles.
Ligament and Tendon Adaptations [edit | edit source]
There is an increase in the cross-sectional area of ligaments and tendons in response to prolonged training, as the insertion sites between ligaments and bones and tendons and bones become stronger.
Metabolic Adaptations of Prolonged Exercise [edit | edit source]
Endurance training:
- Increases the size and number of mitochondria in the trained muscle
- The myoglobin content may sometimes increase, thus the oxygen storage capacity increases.
- Trained muscles glycogen storage capacity increases, and the ability to use fat as an energy source.
Long Term Cardiac Adaptations [edit | edit source]
When healthy individuals participate in a long term aerobic exercise programme they undergo positive cardiac adaptions, both morphologically and physiological.
- Increased early diastolic filling and increased contractile strength.
- Morphological changes appear in both the left ventricle and right ventricle.
- Cardiac adaptations lead to increased cardiac output while exercising, and a higher VO2max after exercise[5]
- Post-training heart rate is decreased at rest and during sub-maximal exercise.
Stroke volume increases through long term endurance training.
- Endurance training increases plasma volume, which elevates the blood volume that returns to firstly the right heart and after that to the left ventricle.
- The greater amount of blood in circulation causes an increase in the amount of blood in the left ventricle when the end-diastolic phase is reached. The end-diastolic phase is the phase in which the passive filling (diastole) of the heart finishes.
- The left ventricle is fully filled and its wall is stretched.
- The passive stored energy in the wall helps to a forceful contraction in the emptying phase (systole).
- As a result, the heart muscle is hypertrophied.
- Each heart muscle fibre increases in size. Hypertrophy refers to the ventricle and the posterior and septal walls.
High blood pressure = systolic blood pressure ≥140 and/or diastolic blood pressure ≥90 mm Hg blood pressure. The positive correlation of blood pressure and cardiovascular disease (CVD) risk starts from 115 mm Hg systolic and 75 mm Hg diastolic and doubles with every 20 mm Hg systolic and 10 mm Hg diastolic increase.
According to the American College of Sports medicine, dynamic aerobic training reduces blood pressure (BP) in individuals with hypertension.
- Hypertension is a risk factor for cardiovascular events.
- Endurance exercises lower arterial blood pressure for some hours after a bout of exercise: this phenomenon is post-exercise hypotension.
- Post-exercise hypotension seems to be greater in people with higher pre-exercise blood pressure values.
- Blood pressure reductions occur after short bouts of exercises of 3 minutes duration and an intensity of 40% VO2max.
- Morphological cardiac adaptations are less in people with cardiovascular disease than when compared to younger, healthy people. [5]
Long Term Respiratory Adaptations [edit | edit source]
The blood flow in the upper regions of the lungs increases after prolonged endurance training and the respiration rate increases.
Absolute Contraindications to Exercise [edit | edit source]

Unstable Cardiovascular Disease (peripheral and central):[6] [7] acute myocardial infarction or unstable angina until stable for at least 5 days, dyspnoea at rest, pericarditis, myocarditis, endocarditis, symptomatic aortic stenosis, cardiomyopathy, unstable or acute heart failure, uncontrolled tachycardia.
- Fever: should be settled to avoid a risk of developing myocarditis.
- Acute pulmonary embolism or pulmonary infarction. Excessive or unexplained breathlessness on exertion.
- Any acute severe illness
- Serious musculoskeletal injury/problem[6]
- Severely impaired cognitive functioning [6]
Precautions with Exercise [edit | edit source]
- Uncontrolled or poorly controlled asthma.
- COPD: Patients are required to be stable before training and oxygen saturation levels should be above 88-90%.
- Cancer or blood disorders: when treatment or disease cause leukocytes below 0.5 x109/L, haemoglobin below 60g/L or platelets below 20 x 109/L.[8] If a patient has a platelet count of <20 000 then only AROM and ADLs are advised due to the increased risk of bleeding, 20 000-30 000: light exercise only.[9]
- Diabetes: If blood glucose is >13 mmol or <5.5 mmol/l then it should be corrected first.8 Patients with severe diabetic peripheral or autonomic neuropathy or foot ulcers should be assessed before undertaking exercise.[10] Cease exercise with diabetes with acute illness or infection.
- Hypertension: resting blood pressures of a systolic >180 or diastolic >100 or higher should receive medication before regular physical activity with particular restrictions on heavyweights strength conditioning, which can create particularly high pressures.
- Osteoporosis: avoid activities with a high risk of falling.
- Unexplained dizzy spells.
Adverse Effects [edit | edit source]
Musculoskeletal Adverse Effects [edit | edit source]
Sudden force development or repetitive movements can lead to musculoskeletal strain, tear or fracture.
Cardiovascular Events [edit | edit source]
In an epidemiological study, the Prevalence of Sudden Cardiac Arrest (SCA) was studied between 2002-2013 and was compared with medical data in the USA.
- Of 1,247 cases of SCA, 63 occurred during sports activities.
- The affected persons were 51.1 ±8.8 years old.
- The incidence is 21.7 (95% -CI 8.1-35.4) per million per year and varies based on sex for sports SCA.
- Men possess a Risk Ratio of 2.58 (95%-CI 2.12-3.13)
Another study investigated the US National Registry of Sudden Death in Athletes. They found
- A total of 2406 deaths between the years 1980-2011.
- The young athletes were 19 ±6 years old and were engaged in 29 diverse sports.
- Young men were affected 6.5 times more frequently than women.
- The most common reason was hypertrophic cardiomyopathy.
References [edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Patel PN, Zwibel H. Physiology, exercise. InStatPearls [Internet] 2019 May 5. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK482280/ (last accessed 16.2.2020)
- ↑ Benjamin Cummings Publishing Co. Factors that affect blood pressure. Available online at:http://www.interactivephysiology.com/demo/misc/assignmentfiles/cardiovascular/Fact_Aff_Blood_Pressure.pdf [Accessed 3 Dec 2018]
- ↑ Joseph T. Wearn. The extent of the capillary bed of the heart. J Exp Med. 1928 Jan 31; 47(2): 273–290.
- ↑ Pescatello LS, Franklin BA, Fagard R, Farquhar WB, Kelley GA, Ray CA; American College of Sports Medicine position stand. Exercise and hypertension.Med Sci Sports Exerc. 2004 Mar;36(3):533-53.
- ↑ 5.0 5.1 Lavie CJ, Arena R, Swift DL, Johannsen NM, Sui X, Lee DC, Earnest CP, Church TS, O'keefe JH, Milani RV, Blair SN. Exercise and the cardiovascular system: clinical science and cardiovascular outcomes. Circulation research. 2015 Jul 3;117(2):207-19.
- ↑ 6.0 6.1 6.2 Spruit MA, Burtin C, De Boever P, Langer D, Vogiatzis I, Wouters EF, Franssen FM. COPD and exercise: does it make a difference?. Breathe. 2016 Jun 1;12(2):e38-49.
- ↑ Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, Hill K, Holland AE, Lareau SC, Man WD, Pitta F. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. American journal of respiratory and critical care medicine. 2013 Oct 15;188(8):e13-64
- ↑ O'Halloran, P and Bhogal, G (Eds). Exercise Medicine for Students: A one-stop resource for the knowledge and promotion of the physical activity. Motivate2Move
- ↑ O'Sullivan SB, Siegelman RP, editors. National Physical Therapy Examination: Review & Study Guide. Therapy Ed; 2021. Available at: https://www.therapyed.com/physical-therapy/review-study-guide [last accessed 9.12.2021]
- ↑ Colberg SR, Sigal RJ, Fernhall B, et al. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: a joint position statement. Diabetes Care. 2010;33(12):e147-67.
Source: https://www.physio-pedia.com/Exercise_Physiology
0 Response to "What Are Training Adaptations to Continued Endurance Exercise Explain Physiologically"
Post a Comment